Support & resources
PANZYGA offers resources to help support patients on their IVIg therapy journey.
The Pfizer Pledge Warranty program*† for adult patients with CIDP starting PANZYGA

As part of its commitment to patients with CIDP, Pfizer is proud to offer the Pfizer Pledge Warranty Program*† for adult patients with CIDP starting PANZYGA. With this program, eligible, adult patients can get their out-of-pocket drug costs for PANZYGA refunded. See below to learn more.
What does the Pfizer Pledge Warranty Program offer?
- With this program, eligible patients can be refunded their out-of-pocket drug costs for up to the first 4 treatments of PANZYGA for chronic inflammatory demyelinating polyneuropathy (CIDP) if the treatment is discontinued by the patient’s healthcare provider for clinical reasons
- Per treatment and aggregate maximum refund limits apply. If the patient’s commercial insurance and/or other payers paid for all or a portion of the cost of PANZYGA, the plan(s) can be refunded those costs up to the program maximum limits minus any out-of-pocket drug costs paid by the patient
Who is eligible for the Pfizer Pledge Warranty Program?
- The Pfizer Pledge Warranty Program is available to adult, cash-paying or commercially insured patients (those with employer-sponsored or private insurance) prescribed PANZYGA for CIDP whose healthcare provider discontinues treatment for clinical reasons before the fifth treatment‡
- Patients are not eligible for the program if their PANZYGA was covered, in whole or in part, by Medicare, Medicaid, TRICARE, Veterans Affairs health care, a state prescription drug assistance program, or the Government Health Insurance Plan available in Puerto Rico
*Not available for residents of Puerto Rico.
†Terms and conditions/eligibility requirements apply. See full terms and conditions at PanzygaInfo.com.
‡Single treatments may be given over 1 or more days.
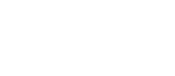
Pfizer Pledge Warranty Program for PANZYGA Downloadable Documents
Patient Warranty Claim Form
Please download, fill out, and submit this form to start the claims process. If you have questions, call 1-800-276-0726 Monday through Friday, 8 AM to 8 PM ET for assistance.
Patient Declarations and Authorizations Forms
Please read, sign, and submit this form. It is needed to process your claim.

Healthcare Provider Attestation Form
Please give this form to your healthcare provider to fill out.
Pharmacy Attestation Form
Please give this form to your specialty infusion pharmacist to fill out.

Terms and Conditions
Pfizer, Inc. (referred to as "us," "we" and similar terms) is proud to offer the Pfizer Pledge Warranty Program for PANZYGA (the "Program") to each Patient (referred to as "you," "your" and similar terms) who meets the Eligibility Requirements and follows the Program Procedures defined below, subject to all the terms and conditions in this document (the "Terms"). You should carefully review these Terms.
Overview of Program
For Patients who meet the Eligibility Requirements, Pfizer will refund the out-of-pocket amount that you paid for up to the first 4 Treatments of PANZYGA for the chronic inflammatory demyelinating polyneuropathy (CIDP) indication, up to a maximum of $16,500 per treatment. The total, per patient, Program refund shall not exceed $50,000 (the “Maximum”). Treatment is defined as the total prescribed dose, which may be administered by a healthcare provider over one or more days. If your commercial insurance and/or other payers (“Your Plan(s)”) paid for all or a portion of the cost of PANZYGA, Pfizer will, on your behalf, refund Your Plan(s) the Average Sales Price as calculated by Pfizer up to the Maximum, less documented out-of-pocket payments provided by you or on our behalf. Payments to all parties must be equal to or less than the cost paid by each party and may reset Your Plan(s)’s out-of-pocket deductible cost in accordance with Your Plan(s)’s benefit design. The order of priority of Warranty payments is first to you and then to Your Plan that is primary and then to Your Plan(s) that are secondary as determined by information provided by you and the documented proof of payment that you provide to us. You are responsible for submitting proof of payment for you and for Your Plan(s). All claims payments will be reported to Your Plan(s).
Medication Eligible for the Program
PANZYGA [Immune Globulin Intravenous (Human) - ifas]
Carton NDC Number Container NDC Number Product Description 00069-1011-02 00069-1011-01 PANZYGA IVIG 1G/10ML SSOL 1X1 VL 00069-1109-02 00069-1109-01 PANZYGA IVIG 2.5G/25ML SSOL 1X1 VL 00069-1224-02 00069-1224-01 PANZYGA IVIG 5G/50ML SSOL 1X1 VL 00069-1312-02 00069-1312-01 PANZYGA IVIG 10G/100ML SSOL 1X1 VL 00069-1415-02 00069-1415-01 PANZYGA IVIG 20G/200ML SSOL 1X1 VL 00069-1558-02 00069-1558-01 PANZYGA IVIG 30G/300ML SSOL 1X1 VL
Eligibility Requirements
The Pfizer Pledge Warranty Program is available to adult, cash-paying or commercially insured patients. Patients are not eligible for the program if their PANZYGA was covered, in whole or in part, by Medicare, Medicaid, TRICARE, Veterans Affairs health care, a state prescription drug assistance program, or the Government Health Insurance Plan available in Puerto Rico. Commercially insured or cash-paying adult patients must satisfy all of the following criteria in order to be eligible to use the Program:
- You are a resident of the 50 United States of America or the District of Columbia. The Program is void for any request made by anyone living outside the 50 United States or the District of Columbia.
- You were prescribed PANZYGA by your healthcare provider to treat chronic inflammatory demyelinating polyneuropathy (CIDP).
- You used PANZYGA on-label according to the instructions provided by your healthcare provider.
- You have not used another Immunoglobulin product in the past 12 months.
- You discontinued PANZYGA for clinical reasons defined at the discretion of the healthcare provider. Discontinuation or switching to another Ig (intravenous or subcutaneous) product due to patient choice, affordability, or for a non-clinical reason does not qualify for the Program.
- You must discontinue using PANZYGA prior to the administration of the fifth treatment of PANZYGA.
- PANZYGA treatment administered as a hospital inpatient is not eligible for the Warranty.
- You are not eligible to participate in this Program if you are enrolled in a state or federally funded insurance program, including but not limited to Medicare, Medicaid, TRICARE, Veterans Affairs health care, a state prescription drug assistance program, or the Government Health Insurance Plan available in Puerto Rico (formerly known as “La Reforma de Salud”).
- Your first treatment of PANZYGA must be administered on or after July 1, 2022, and on or before June 30, 2023 (the “Coverage Period”).
- Only PANZYGA sold by Pfizer will be eligible for this warranty. You may be able to identify this through the NDC codes listed in the “Medication Eligible for the Program” section.
Costs other than for the drug will not be reimbursed (i.e., administration costs).
You must submit all Claims Information (as described below) within 180 days following the administration date of your last treatment of PANZYGA.
Benefit Request Process
- To be eligible for a refund under this Program, you must satisfy the requirements and submit the information below (the “Claims Information”), 180 days following the date of your last treatment of PANZYGA. Call 1-800-276-0726 and a representative will provide you with a Patient Warranty Claim Form, a Patient Declarations and Authorizations Form, a Healthcare Provider Attestation Form, and a Pharmacy Attestation Form, or these forms may be downloaded from www.panzygainfo.com.
- You will need to provide a copy/photo of the following: (1) both sides of your insurance card(s) for both prescription and medical benefit insurance, (2) the Explanation of Benefits (EOB) for each treatment from your Health Insurer(s).
- You will then need to return a fully completed and signed (1) Patient Warranty Claim Form, (2) Patient Declarations and Authorizations Form, (3) Healthcare Provider Attestation Form, and (4) Pharmacy Attestation Form in accordance with their instructions, which will include the following information:
- Patient Warranty Claim Form:
- Your name, date of birth, phone number, address, gender, and email address
- Prescribing healthcare provider name, phone number, and address
- For each treatment, the dispensing pharmacy name, phone number, and address
- For each treatment, Your Plan(s)’s information and amounts paid by Your Plan(s), including the following:
- For each primary insurer, secondary insurer and prescription insurer: the insurance type, insurer name, phone number, address, policy beneficiary ID number, group number, policyholder name, policyholder relationship, and policyholder date of birth
- Patient Declarations and Authorizations Form, which includes your:
- Consent for the Pfizer Pledge
- Consent to receive communication from our representative to process your claim
- Authorization to share health information to process your claim
- Acknowledgment of laws
- Healthcare Provider Attestation Form, completed and signed by your prescribing healthcare provider, which includes the following information:
- Your name and date of birth
- Prescribing healthcare provider name, phone number and address
- Prescribing healthcare provider’s attestation that PANZYGA was prescribed for on-label use for the chronic inflammatory demyelinating polyneuropathy (CIDP) indication, and the clinical rationale for discontinuance of PANZYGA (no confirmatory documentation required)
- Attestation that you have discontinued PANZYGA prior to the fifth treatment of PANZYGA
- Pharmacy Attestation Form, completed and signed by the pharmacy dispensing PANZYGA or the clinic infusing PANYZGA, which includes the following information:
- Your name and date of birth
- The PANZYGA treatment dates
- The number of vials of each strength of PANZYGA dispensed for each treatment date
- For each treatment date: the amount of money you paid out-of-pocket, the amount of financial assistance from the Pfizer PANZYGA Co-Pay Program, and the amount of co-pay assistance from any other source other than the Pfizer PANZYGA Co-pay Program
- The number of Pfizer vials of PANZYGA that were dispensed (Pharmacy) or infused (Clinic)
- The amount of money documented on the form was collected
- Federal programs (including but not limited to Medicare, Medicaid, TRICARE, Veterans Affairs health care, a state prescription drug assistance program, or the Government Health Insurance Plan available in Puerto Rico (formerly known as “La Reforma de Salud”) were not billed for PANZYGA
- If your Claims Information passes the verification process, we will notify you via telephone or email that you have been approved for coverage.
- If your Claims Information does not pass the verification process, we will notify you via email that your request has been denied and the email will include the reason for the denial (such as incomplete information, mismatched information, etc.). You will be given the opportunity to resubmit your Claims Information within 30 days of the email notification.
Additional Terms and Conditions
By submitting your Claims Information under the Program, you are representing and warranting that you took the medication in accordance with the instructions that were provided by your prescribing healthcare provider.
- We reserve the right to modify the processes, procedures, parameters, or other terms of the Program, or terminate the Program entirely, at any time, without prior notice to you. If we terminate the Program, we will: continue to honor valid warranty claims for patients whose initial dose of PANZYGA occurred prior to the termination date of the program. The current status of the Program and applicable terms are available at www.panzygainfo.com
- We are refunding payments under this Program to you and Your Plan(s) based on the information provided by you. You are responsible for resolving any disagreements related to reimbursements made by us, on Your behalf, to Your Plan(s)
LIMITATION OF LIABILITY
IN NO EVENT, UNDER ANY CAUSE OF ACTION OR THEORY OF LIABILITY, SHALL PFIZER, ITS DISTRIBUTORS OR SUPPLIERS BE LIABLE TO YOU OR ANY THIRD PARTY FOR ANY INDIRECT, INCIDENTAL, CONSEQUENTIAL, SPECIAL, EXEMPLARY, OR PUNITIVE DAMAGES, OF ANY NATURE WHATSOEVER, ARISING OUT OF OR IN CONNECTION WITH THE PROGRAM, EVEN IF PFIZER HAS BEEN ADVISED OF THE POSSIBILITY OF SUCH DAMAGES.
NOTWITHSTANDING ANY DAMAGES THAT YOU MIGHT INCUR FOR ANY REASON WHATSOEVER, INCLUDING, WITHOUT LIMITATION, ALL DAMAGES REFERENCED HEREIN AND ALL DIRECT OR GENERAL DAMAGES IN CONTRACT, TORT (INCLUDING NEGLIGENCE) OR OTHERWISE, THE ENTIRE AGGREGATE LIABILITY OF PFIZER AND ANY OF ITS DISTRIBUTORS AND/OR SUPPLIERS SHALL BE LIMITED TO THE MAXIMUM AMOUNT SET FORTH ABOVE FOR THE PRODUCT THAT IS SUBJECT TO THE PROGRAM. SOME STATES AND/OR JURISDICTIONS DO NOT ALLOW THE EXCLUSION OR LIMITATION OF INCIDENTAL OR CONSEQUENTIAL DAMAGES, SO THE ABOVE LIMITATIONS OR EXCLUSIONS MAY NOT APPLY TO YOU. THE LIMITATIONS OF LIABILITY SET FORTH ABOVE SHALL APPLY TO THE MAXIMUM EXTENT PERMITTED UNDER APPLICABLE LAW.
ARBITRATION: Read the following arbitration provision (“Provision”) carefully. It limits certain of your rights, including your right to obtain relief or damages through court action.
To begin Arbitration, either you or we must make a written demand to the other party for Arbitration for the applicable claim ("Claim"). The Arbitration will take place before a single arbitrator. It will be administered in keeping with the Expedited Procedures of the Commercial Arbitration Rules ("Rules") of the American Arbitration Association ("AAA") in effect when the Claim is filed. You may get a copy of the AAA's Rules by visiting www.adr.org. The filing fees to begin and carry out Arbitration will be shared equally between you and us. This does not prohibit the arbitrator from giving the winning party their fees and expenses for the Arbitration. Unless you and we agree, the Arbitration will take place in the county and state where you live. The Federal Arbitration Act, 9 U.S.C. Ch. 1, et seq., will govern, and not any state law on Arbitration. YOU AGREE AND UNDERSTAND THAT this Arbitration Provision means that you give up your right to go to court on any Claim covered by this provision. You also agree that any Arbitration proceeding will only consider your Claim. Claims by, or on behalf of, other individuals will not be arbitrated in any proceeding that is considering your Claim. THE DEGREE TO WHICH ARBITRATION CAN BE USED AS A DISPUTE RESOLUTION PROCESS FOR CONSUMER CLAIMS VARIES FROM STATE TO STATE, SO THIS ARBITRATION PROVISION MAY NOT APPLY TO YOU, DEPENDING ON YOUR STATE OF RESIDENCE. In the event this Arbitration provision is not approved by the appropriate state regulatory agency, and/or is stricken, severed, or otherwise deemed unenforceable by a court of competent jurisdiction, you and we specifically agree to waive and forever give up the right to a trial by jury. Instead, in the event any litigation arises between you and us, any such lawsuit will be tried before a judge, and a jury will not be impaneled or struck.
If you have been prescribed PANZYGA and have questions about your coverage, call Pfizer IGuide™ Monday through Friday, 8 AM to 8 PM ET, at 1-844-448-4337.
Financial Assistance
- Pfizer IGuide™ can help identify financial assistance resources for which you may be eligible to help with out-of-pocket costs for PANZYGA
Commercially Insured Patients
- If you have commercial, employer, or private coverage, including coverage purchased through a state health insurance marketplace, you may be eligible for the PANZYGA Co-Pay Program, which can help cover the cost of your co-pay. Eligible patients may pay as little as $0 per PANZYGA treatment. The value of the co-pay card is limited to a maximum of $5,000 per calendar year. See terms and conditions below
Medicare/Government-Insured Patients
- If you have government-funded insurance and need help to cover the cost of PANZYGA, Pfizer IGuide™ can help identify financial support options including alternate coverage resources, if available
Uninsured Patients
- If you do not have health insurance and cannot afford your PANZYGA treatment, Pfizer IGuide™ can connect you to potential resources that may help cover the cost of PANZYGA, including how to apply to Medicaid if you may be eligible
Eligible patients can save with the Pfizer PANZYGA Co-Pay Program
Eligible, commercially insured patients can receive assistance of up to $5,000* per calendar year or the cost of the patient’s co-pay in a 12-month period (whichever is less) for claims received by the program.
![]() Contact your specialty infusion pharmacy to see if you are eligible.
Contact your specialty infusion pharmacy to see if you are eligible.
*Terms and conditions apply. See full terms and conditions below. All specialty infusion pharmacies may participate in the PANZYGA co-pay assistance program. Eligible, commercially insured patients can receive co-pay assistance up to $5,000 per calendar year.
Eligibility requirements
- Patients must have commercial insurance to be eligible
- Patients are not eligible if they are enrolled in a state or federally funded insurance program
For eligible patients prescribed PANZYGA, the co-pay program is available through specialty infusion pharmacies.
The Pfizer PANZYGA Co-Pay Program Terms and Conditions for Patients
TERMS AND CONDITIONS
By using this co-pay card, you acknowledge that you currently meet the eligibility criteria and will comply with the terms and conditions described below:
- Patients are not eligible to use this card if they are enrolled in a state or federally funded insurance program, including but not limited to Medicare, Medicaid, TRICARE, Veterans Affairs health care, a state prescription drug assistance program, or the Government Health Insurance Plan available in Puerto Rico (formerly known as “La Reforma de Salud”).
- Patient must have private insurance. Offer is not valid for cash paying patients. The value of this co-pay card is limited to a maximum of $5,000 per calendar year or the cost of patient co-pay in a 12-month period, whichever is less.
- This co-pay card is not valid when the entire cost of your prescription drug is eligible to be reimbursed by your private insurance plan or other private health or pharmacy benefit programs.
- You must deduct the value of this co-pay card from any reimbursement request submitted to your private insurance plan, either directly by you or on your behalf.
- You are responsible for reporting use of the co-pay card to any private insurer, health plan, or other third party who pays for or reimburses any part of the prescription filled using the co-pay card, as may be required. You should not use the co-pay card if your insurer or health plan prohibits use of manufacturer co-pay cards.
- Patient must be 2 years of age or older to be eligible for the co-pay benefit.
- Co-pay card cannot be combined with any other savings, free trial or similar offer for the specified prescription.
- Co-pay card will be accepted only at participating pharmacies.
- If your pharmacy does not participate, you may be able to submit a request for a rebate in connection with this offer.
- This co-pay card is not health insurance.
- Offer good only in the U.S. and Puerto Rico.
- Co-pay card is limited to 1 per person during this offering period and is not transferable.
- A co-pay card may not be redeemed more than once per 13 days per patient.
- No other purchase is necessary.
- No membership fee.
- Data related to your redemption of the co-pay card may be collected, analyzed, and shared with Pfizer for market research and other purposes related to assessing Pfizer’s programs. Data shared with Pfizer will be aggregated and de-identified; it will be combined with data related to other co-pay card redemptions and will not identify you.
- Pfizer reserves the right to rescind, revoke or amend this offer without notice.
- Offer expires 12/31/2023.
For more information, call 1-866-642-7606, visit https://panzyga.pfizerpro.com/support/co-pay-program-for-patients, or write:
Panzyga Co-Pay Program
P.O. Box 6875
Bridgewater, NJ 08807
Resources for you throughout your treatment
Back to topPANZYGA offers a variety of downloadable resources with information about treatment, including guides to keep track of your therapy. To view the Full Prescribing Information in English, click here. To view the Full Prescribing Information in Spanish, click here.
Downloadable patient materials

PANZYGA CIDP brochure
View Full Prescribing Information, including complete BOXED WARNING.
What to Expect From Your IVIg Therapy brochure
View Full Prescribing Information, including complete BOXED WARNING.
PANZYGA therapy tracker
View Full Prescribing Information, including complete BOXED WARNING.
Pfizer PANZYGA co-pay program brochure
View Full Prescribing Information, including complete BOXED WARNING.

PANZYGA digital resource guide
View Full Prescribing Information, including complete BOXED WARNING.

PANZYGA CIDP warranty program overview
View Full Prescribing Information, including complete BOXED WARNING.
Video library

PANZYGA Co-Pay Program Video
View Full Prescribing Information, including complete BOXED WARNING.
PANZYGA CIDP Brochure Video
View Full Prescribing Information, including complete BOXED WARNING.

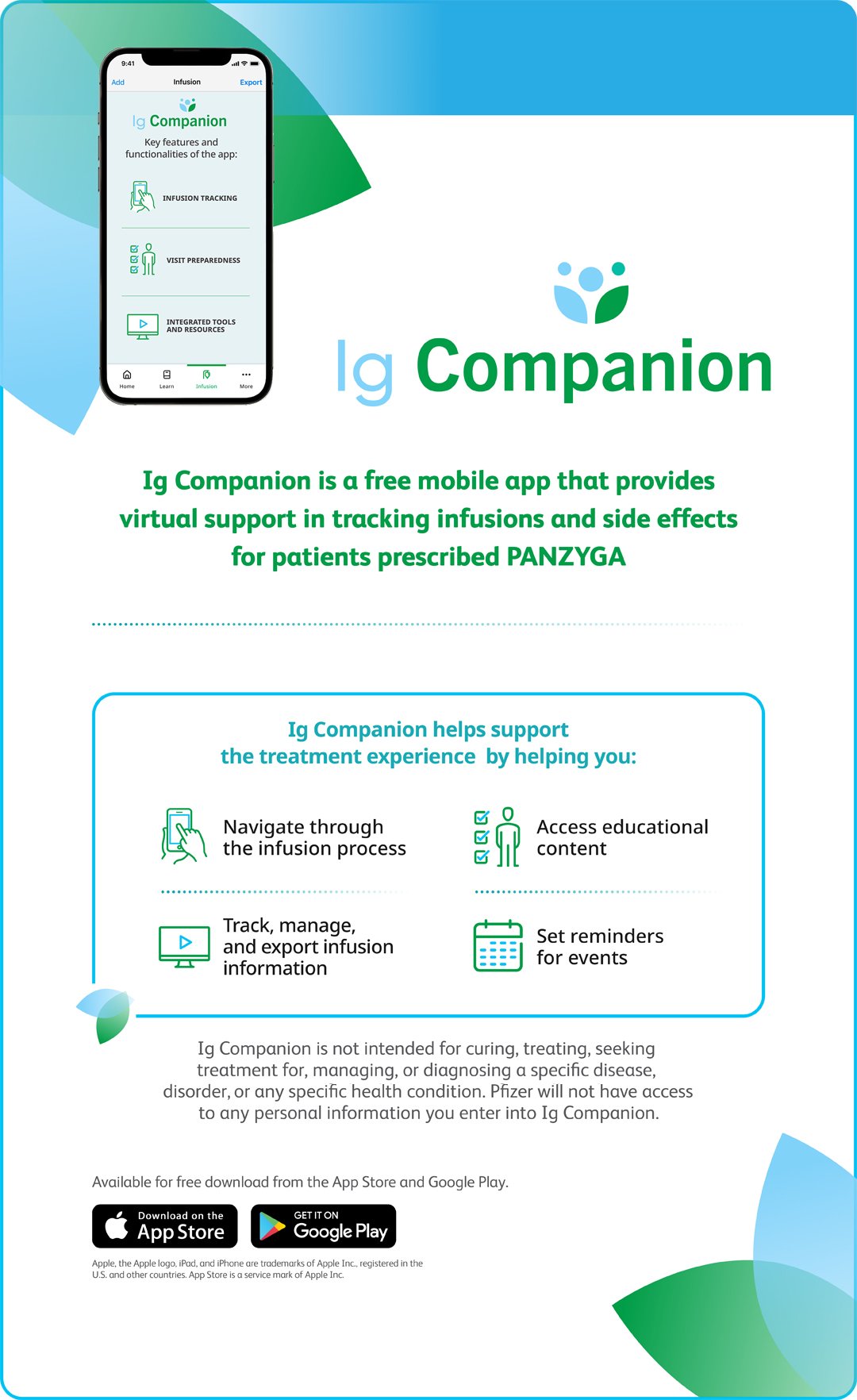
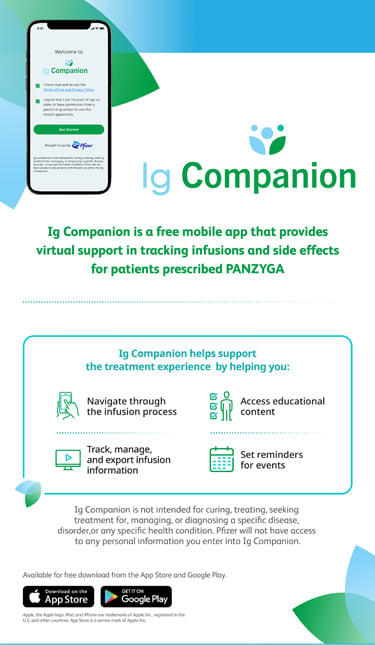
Ig Companion overview video
View Full Prescribing Information, including complete BOXED WARNING.
What to Expect From Your IVIg Therapy video
View Full Prescribing Information, including complete BOXED WARNING.

Pfizer CIDP warranty program video
View Full Prescribing Information, including complete BOXED WARNING.
Frequently asked questions
Back to topWhat is PANZYGA?
PANZYGA is a liquid medicine for infusion that contains immunoglobulin G (IgG). It is made from human plasma that is donated by healthy people and contains antibodies that replace the missing antibodies in patients with PI or cITP. In patients with CIDP, these antibodies block the body from attacking its own nerve cells.
What should I know before taking PANZYGA?
- PANZYGA can make vaccines (like measles/mumps/rubella or chickenpox vaccines) work less effectively for you. Before you get any vaccines, tell your healthcare provider that you take PANZYGA
- Decreased kidney function and kidney function failure can occur
- Severe headache, drowsiness, fever, painful eye movements, or nausea and vomiting can occur
- Elevated blood pressure can occur particularly in patients who have a history of hypertension (high blood pressure)
- If you are elderly, with heart or kidney problems, discuss with your healthcare provider prior to initiating treatment with PANZYGA
- PANZYGA is made from human blood and therefore may have a risk of transmitting infectious agents, including viruses and, theoretically, the variant Creutzfeldt-Jakob disease (CJD) and CJD agent. The production and manufacturing process reduces this risk, but the risk cannot be eliminated
How are PANZYGA treatments given?
PANZYGA is in a class of medicine called intravenous immunoglobulin (IVIg) therapy. PANZYGA is given as an infusion through a small needle in a vein administered by a healthcare provider. Your infusion will start at a slow rate. It may gradually increase if you tolerate it well. That is why your healthcare provider will monitor you during your infusion. They will be looking for signs of infusion reactions. These reactions can include headache, abdominal pain, fever, nausea, fatigue, vomiting, dizziness, and anemia. They may stop your PANZYGA treatment if you experience a severe reaction. Slowing or stopping the infusion may help these symptoms to go away.
What were the results of the clinical studies of PANZYGA?
In a clinical study of adult patients with CIDP who received PANZYGA:
- In the group of 69 patients treated with 1 g/kg of PANZYGA, 80% of patients improved
- PANZYGA was also tested at a higher dose of 2 g/kg in 36 patients. 92% of patients who received the 2 g/kg dose of PANZYGA improved
In a clinical study of patients aged 2 years or older with PI who received PANZYGA:
- In a clinical study, PANZYGA helped prevent serious bacterial infections (SBIs) in people with PI. In a group of 51 patients treated with PANZYGA at a dose between 200 and 800 mg per kg body weight every 3 or 4 weeks, a total of 50 patient-years were studied and 4 SBIs were observed
In a clinical study of adult patients with cITP who received PANZYGA:
- In a clinical study, PANZYGA helped increase platelets (a type of blood cell) and decrease bleeding in patients with cITP. In a group of 36 patients treated with PANZYGA at a dose of 2 g/kg body weight administered as 2 daily 1 g/kg doses given on 2 consecutive days, approximately 81% (29 of 36) patients responded to PANZYGA with an increase in platelet count within 7 days of treatment
What are the most common side effects seen with PANZYGA?
- For adults with CIDP, the most common adverse reactions during a clinical trial were: headache, fever, skin irritation, and blood pressure increase
- For people 2 years of age and older with PI, the most common adverse reactions during a clinical trial were: headache, abdominal pain, fever, nausea, sinusitis, fatigue, and bronchitis
- For adults with cITP, the most common adverse reactions during a clinical trial were: headache, fever, nausea, vomiting, dizziness, and anemia
How can I keep track of my PANZYGA treatments?
It is important to keep an infusion journal to record details of each PANZYGA infusion, so that your healthcare provider can monitor your progress. Be sure to fill out every section and keep an accurate record of each time your PANZYGA is administered. Please remember to bring your tracker to any appointments with your healthcare provider. During your first few infusions, it is recommended that you ask your infusion nurse or trainer to help you complete your tracker.
Download the PANZYGA Therapy Tracker to keep track of when you receive PANZYGA.
To download the Full Prescribing Information including complete BOXED WARNING in English, click here.
To download the Full Prescribing Information including complete BOXED WARNING in Spanish, click here.
How long does it take to infuse PANZYGA?
For adult patients with CIDP who receive PANZYGA:
- Your first PANZYGA infusion will take the most time
- Your other PANZYGA infusions may last several hours
For patients aged 2 years or older with PI who receive PANZYGA:
- Your first PANZYGA infusion will take the most time
- Your other PANZYGA infusions may last between 1¼ and 2 hours
For adult patients with cITP who receive PANZYGA:
- Your first PANZYGA infusion will take the most time
- Your other PANZYGA infusions may last about 3 hours